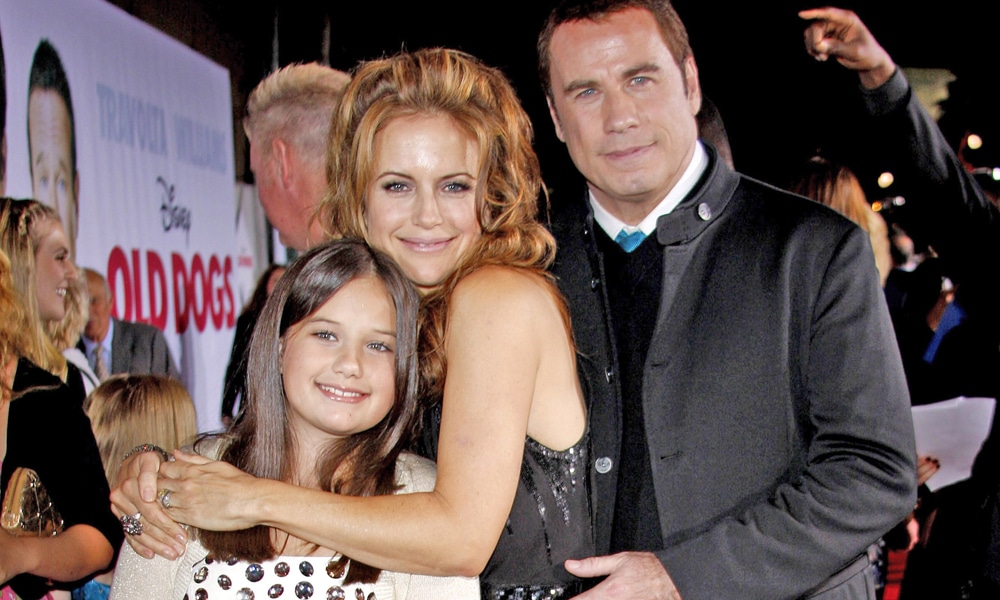
The death of Kelly Preston yesterday took all of us – except for those closest to her – by surprise. When a vibrant, beloved soul leaves this world all too soon, we must pause to respect the brevity and ultimate fragility of life. To that end, self-care matters so very much. This is a reminder for us to control whatever we can when it comes to breast cancer. Early detection and maximal risk reduction remain our best defenses against this killer disease that affects 1 in 8 US women (12.5 percent), takes the lives of 1 in 39 US women (3 percent), and will claim approximately 41,760 women and 500 men this year alone.
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
![]()
Only two years passed between Preston’s diagnosis and death. How can this happen, and happen so quickly? The truth is, some breast cancers are more difficult to cure than others, and treatments don’t work in every patient or sometimes work for a while and then stop working. When a woman dies from breast cancer in a short timeframe, this means her cancer was diagnosed at Stage IV (more on that later), and the cancer subtype was likely biologically aggressive, such as “triple negative” or “inflammatory” breast cancers tend to be.
Did Her Pregnancy At Age 48 Play A Role?
For those wondering about Kelly Preston’s pregnancy at age 48 and how that might have contributed to her cancer, note the following facts:
- It is true that those who wait until age thirty-five or older for a first full-term pregnancy carry a 40 percent increase in breast cancer compared to women without kids.[1] The good news, however, is that this elevated risk only lasts for ten to fifteen years and then drops below that of the never-pregnant woman. And anyways, her first full-term pregnancy was at age 30.
- Pregnancy potentially promotes a temporary increase in breast cancer growth, since pregnancy hormones can fuel existing cancer cells (present pre-pregnancy but undetected), but then, these same women enjoy a long-term protective effect since pregnancy also causes some breast cells to resist carcinogenic stimuli.[2] So yes, there can be a post-pregnancy bump in estrogen-driven breast cancer, but that cancer already existed.
- It is true that older childbearing women demonstrate a slight increase in breast cancer relative to their never-pregnant peers, but this is for reason #2 above, and is temporary.[3]
- A multitude of studies conclude that prospective moms using any of the ovarian stimulation medications associated with boosting fertility or undergoing IVF, including clomiphene citrate (Clomid), gonadotropin-releasing hormone (GnRH antagonist, Lupron), human chorionic gonadotropin (hCG), follicle stimulating hormone (FSH), luteinizing hormone (LH), and progesterone, do not have a higher risk of breast cancer.[4] In fact, it might be lower.
To summarize: Preston’s later-age pregnancy with baby Ben had no causative relationship to her breast cancer.
Over 11 hours of video content are now available to stream from any device. If you cannot attend our annual Summit at Terranea Resort, sign up for the Virtual Summit instead and get the same information from the in-person Summit in the convenience of your own home.
Quick Facts About Metastatic Breast Cancer
More than 3.8 million US women with a history of breast cancer are alive today, whether cancer-free or undergoing treatment.[5] Knowing that stage I cancers have a 99 percent 5-year survival rate might create a false sense of cancer curability. The truth is, despite our best efforts, about 25 percent of women initially diagnosed with early-stage breast cancer (that is, not stage IV) eventually develop metastatic disease to a distant organ; but remember, increasingly effective therapies and earlier detection continue to improve this number.[6] Approximately 155,000 women in the United States are alive today with metastatic breast cancer (MBC), which means that cancer cells have metastasized beyond the breast and nearby axillary nodes to other organs or distant nodes, making them stage IV. The most commonly involved areas are lung, liver, brain, and bone. At the time of diagnosis, 6 percent of breast cancers will already have metastasized and be stage IV. While over 11 percent of MBC patients survive more than ten years, the majority (73 percent) will unfortunately live less than five years.[7]
Stay Connected
Stay Connected
For those newly diagnosed with MBC, their treatment team will run a number of tests to understand the extent of spread and the subtype of cancer cells that exist (which could differ slightly from the initial cancer type). Next, they will aim targeted drugs, systemic chemotherapy, immunotherapy, and/or endocrine therapies directly at these rogue cells. Surgery and radiation might be used to control local symptoms like pain, or perhaps to eliminate a solitary tumor site, but with MBC we have to expect micrometastatic cells are in the bloodstream, and therefore, we need to get after them with systemic treatments (not surgery). We have a number of tricks in our armamentarium, so no one should give up hope easily.
Dr. Funk’s “Beat It, Breast Cancer” Checklist
There are ways to improve both health and quality of life with MBC by making lifestyle decisions that are under your control, and importantly so, these very same lifestyle decisions have been scientifically shown to significantly reduce breast cancer risk for women across all ages who wish to do whatever they can to keep disease at bay. The following checklist from Breasts: The Owner’s Manual provides a roadmap for what you can do today to reduce your risk:
- Whole food, plant-based eating that prioritizes vegetables, fruits, 100 percent whole grains, and legumes (beans, peas, lentils), whole food soy, ground flaxseed; eliminate all meat, poultry, fish, dairy, and eggs; minimize saturated fat, simple sugars, processed foods, and refined cereals. If you are new to this way of eating, start slowly by making this Antioxidant Smoothie recipe daily, and then build up from there.
- Exercise: 5 hours a week moderate effort, or 2.5 hours a week vigorous, sweaty workouts.
- Get to your ideal weight and stay there.
- Minimize or eliminate alcohol: 7 drinks or fewer a week, favor 4 to 8 ounces of red wine.
- No smoking.
- Stress management techniques: 20 minute daily minimum (prayer, meditation, tai chi, yoga, guided imagery, focused breathing).
- Social connectedness: 30 minute daily minimum (no screens when with others in person). Examples: date night, coffee with a friend, church group, tennis team, uplifting online community, bridge club.
- Monthly breast self-exam, annual clinical breast exam, annual mammogram, plus additional imaging (ultrasound, MRI) and clinical exams when indicated.
- Extra credit: Give back. Smile. Laugh.
Survived by her children and husband John Travolta, Kelly Preston will be remembered by many for the friendships she shared with them, and by others for her vibrant personality or acting prowess. Our hope should also be that she will remind us of the importance of love and preserving life as best we can.
As always, please leave a comment below if you have any questions. I look forward to hearing from you and wish you the breast of health!
References
- B. MacMahon et al., “Age at First Birth and Breast Cancer Risk,” Bulletin of the World Health Organization 43, no. 2 (1970): 209–21.
- B. MacMahon, “Reproduction and Cancer of the Breast,” Cancer 71, no. 10(1993): 3185–88.
- P. Bruzzi et al., “Short Term Increase in Risk of Breast Cancer After Full Term Pregnancy,” British Medical Journal 297, no. 6656 (October 1988): 1096–98.
- C. Fei et al., “Fertility Drugs and Young-Onset Breast Cancer: Results from the Two Sister Study,” Journal of the National Cancer Institute 104 (2012): 1021–27; L. G. Liat et al., “Are Infertility Treatments a Potential Risk Factor for Cancer Development? Perspective of 30 Years of Follow-Up,” Gynecological Endocrinology 28, no. 10 (2012): 809–14; L. M. Stewart et al., “In Vitro Fertilization and Breast Cancer: Is There Cause for Concern?” Fertility and Sterility 98, no. 2 (2012): 334–40; A. N. Yli-Kuha et al., “Cancer Morbidity in a Cohort of 9,175 Finnish Women Treated for Infertility,” Human Reproduction 27, no. 4 (2012): 1149–55; L. A. Brinton et al., “In Vitro Fertilization and Risk of Breast and Gynecologic Cancers: A Retrospective Cohort Study Within the Israeli Maccabi Healthcare Services,” Fertility and Sterility 99, no. 5 (2013): 1189–96; T. N. Sergentanis et al., “IVF and Breast Cancer: A Systematic Review and Meta-analysis,” Human Reproduction Update 20, no. 1 (2013): 106–23; A. Q. van den Belt-Dusebout et al., “Ovarian Stimulation for In Vitro Fertilization and Long-Term Risk of Breast Cancer,” Journal of the American Medical Association 316, no. 3 (2016): 300–312.
- Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019:1-23.
- J. O’Shaughnessy, “Extending Survival with Chemotherapy in Metastatic Breast Cancer,” Oncologist 10, no. 3 (2005): 20–29; S. Saadatmand et al., “Influence of Tumour Stage at Breast Cancer Detection on Survival in Modern Times: Population-Based Study in 173,797 Patients” BMJ 351 (2015): h4901; B. Gerber, M. Freund, and T. Reimer, “Recurrent Breast Cancer: Treatment Strategies for Maintaining and Prolonging Good Quality of Life,” Deutsches Arzteblatt International 107, no. 6 (2010): 85–91; Nick Mulcahy, “The Mystery of a Common Breast Cancer Statistic,” Medscape, August 18, 2015, https://www. medscape.com/viewarticle/849644#vp_1.
- https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf